Keratoconus is a challenging eye condition that can lead to significant visual impairment, characterized by halos, glare, and overlapping vision. When keratoconus is severe, it may require a corneal transplant. However, there is a new surgical method called Corneal Tissue Addition Keratoplasty (CTAK) that offers hope for patients with keratoconus.
This procedure was invented at the Cornea and Laser Eye Institute, and the first clinical trials for the CTAK procedure began in 2016. CTAK has proven safe, effective, and one of the most exciting procedures developed for keratoconus management. It uses a custom-shaped irradiated corneal tissue, which is added to the patient’s cornea through a channel created by the femtosecond laser, which induces reshaping of the cornea and improved vision.
In this article, we will explore what is CTAK, how it works, and the benefits it provides for patients. We will delve into the results of clinical trials and discuss this innovative procedure to improve visual acuity and corneal topography.
What is CTAK?
CTAK, or Corneal Tissue Addition Keratoplasty, is a surgical procedure designed to address the visual and structural abnormalities caused by keratoconus. It involves the placement of a customized preserved corneal tissue obtained from an eye bank into the patient’s own cornea. The goal of CTAK is to reduce the irregularity of the keratoconic cornea, thereby improving visual acuity. This technique utilizes patient-specific laser-cut cornea tissue, which is gamma-irradiated for sterility and stability.
How Does CTAK Work?
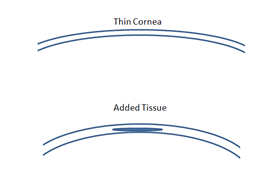
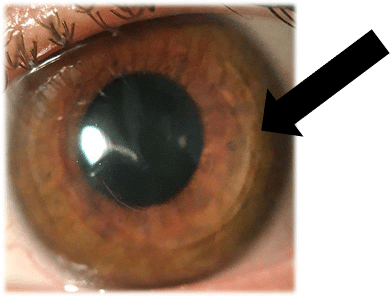
The CTAK procedure begins with the preparation of the corneal tissue. CTAK tissue is processed on a femtosecond laser, which cuts it into a customized shape to ameliorate the patient’s specific corneal map. The tissue is then placed in the patient’s cornea within a channel created by the femtosecond laser. The surgical plan is carefully designed to provide optimal tissue placement. The customized tissue shape ensures a natural and stable flattening of the cornea. The tissue itself is clear and biocompatible.
Clinical Trial Results
Clinical trials evaluating the efficacy of CTAK have shown excellent results for patients with keratoconus. In a single-center, prospective, open-label clinical trial, 21 eyes of 18 patients underwent CTAK. The study measured various visual and topographic parameters before and after the procedure.
The results demonstrated significant improvements in uncorrected distance visual acuity, glasses corrected distance visual acuity, and change in glasses prescription. On average, patient uncorrected vision improved by about 5 logMAR lines (from 1.21 logMAR lines (20/327) to 0.61 logMAR lines (20/82)), vision in glasses improved by over 3 logMAR lines (from 0.62 logMAR lines (20/82) to 0.34 logMAR lines (20/43)), and patient glasses prescriptions improved (from -6.25 diopters to -1.61 diopters).
Individual outcomes were also remarkable, with 95.2% of eyes gaining more than 2 lines of vision without glasses, and 47.6% gaining more than 6 lines. Additionally, 57.1% of eyes gained at least 2 lines of vision with glasses. The topographic analysis showed a significant flattening of the cornea, with an average decrease of -8.4 D in Kmean and -6.9D in Kmax at 6 months after the procedure.
Advantages of CTAK
CTAK offers several advantages over traditional treatment options for keratoconus, such as corneal transplantation and intracorneal ring segments (Intacs). First and foremost, it is a less invasive alternative to corneal transplantation. While corneal transplantation may be necessary in advanced cases of keratoconus, particularly when dense scarring is present, CTAK can provide significant improvements in visual acuity and corneal topography without the long recovery and potential complications associated with a transplant. Additionally, CTAK tissue is irradiated which reduces the risk of rejection compared to full corneal transplants. Another advantage of CTAK is biocompatibility. This tissue is more natural when placed in a patient’s cornea compared to synthetic intracorneal ring segments and inlays.
CTAK tissue is prepared from the stromal tissue of donor cornea. CTAK maximizes the potential of each donation and honors the gift of organ donation by allowing eye banks to use one tissue donation to be divided for the benefit of multiple patients – one for an endothelial transplant (back surface of the cornea) and second for CTAK tissue.
Additionally, CTAK allows for personalized surgical plans tailored to each patient’s specific needs (see figure below). The customization of the tissue ensures a precise and optimal outcome. This personalized approach enhances the effectiveness of the procedure.

How is CTAK Different from CAIRS?
CTAK is not the same as CAIRS. CTAK is a form of lamellar keratoplasty and CTAK tissue is gamma irradiated and fully customized in shape by a femtosecond laser to ameliorate a patient’s individual corneal shape. CAIRS (Corneal Allogenic Intrastromal Ring Segments) was developed to mimic synthetic intrastromal corneal ring segments such as Intacs but made out of corneal tissue for improved biocompatibility.
CTAK Reviews
Conclusion
CTAK represents a significant advancement in the treatment of keratoconus. Its ability to improve visual acuity, corneal topography, and patient quality of life makes it a promising option for individuals with this challenging eye condition. CTAK offers hope for individuals with keratoconus by providing a less invasive and personalized approach to improve visual acuity and corneal topography. This procedure is a potential option for patients who have previously been told that corneal transplant was their only surgical option. This innovative procedure maximizes the potential of donated corneal tissue and has revolutionized the treatment of keratoconus.



