Keratoconus is a progressive eye condition that affects the shape of the cornea, leading to distorted and blurred vision. It typically develops during adolescence or early adulthood and can worsen over time if left untreated. In this comprehensive guide, we will delve into the causes, symptoms, and diagnosis of keratoconus, explore treatment options, and provide tips for managing this condition in everyday life.
What is Keratoconus?
Keratoconus is an eye disease characterized by thinning and bulging of the cornea, the clear front surface of the eye. Keratoconus occurs when the collagen tissue that makes up the cornea weakens. As a result, the cornea begins to stretch and thin, becoming cone-shaped rather than dome-shaped. This can cause visual distortions, and as the disease progresses, scarring and other serious issues.
Keratoconus Causes: Is it Genetic?
The exact cause of keratoconus is still unknown, but it is believed to be a combination of genetic and environmental factors. People with keratoconus often have a family history of the condition, and certain external factors such as eye rubbing and chronic eye irritation may contribute to its development. Additionally, certain systemic conditions such as Down syndrome and connective tissue disorders have been associated with an increased risk of keratoconus.
Exploring the Symptoms of Keratoconus
The symptoms of keratoconus can vary from person to person and may change over time. In the early stages, individuals may experience mild blurring and distortion of vision, which can progress to more severe visual impairment as the condition advances. Other common symptoms include increased sensitivity to light, and the appearance of glare and halos around lights. Some individuals may also notice frequent changes in their prescription glasses or contact lenses, as the irregular shape of the cornea affects the way light enters the eye. Other individuals may notice or be told that their vision does not correct to 20/20 with glasses or contact lenses.
Diagnosing Keratoconus: What to Expect
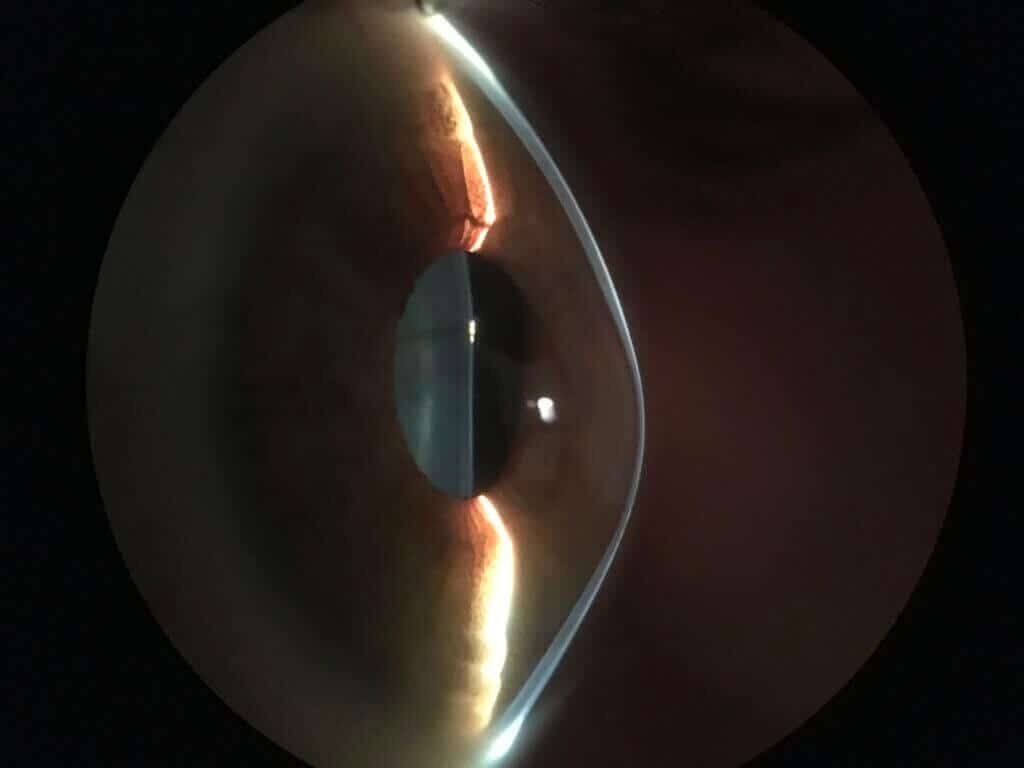
Keratoconus occurs in about one out of every 725 individuals and is notoriously difficult to diagnose. If you are experiencing symptoms of keratoconus or have a family history of the disease, it is important to seek a professional diagnosis from an eye care specialist. Early detection is key to halting the progression of this sight threatening disease. During the diagnostic process, the eye care specialist will perform a comprehensive eye examination, which may include a visual acuity test, corneal topography (mapping), and a slit-lamp examination. These tests will help determine the shape and thickness of your cornea and assess the severity of the condition.
Treatment Options for Keratoconus
Many people wonder if keratoconus can be cured. Currently there is no cure for keratoconus, however, several treatment options are available to manage the condition and improve vision. For example, corneal cross-linking is an effective treatment that can help halt the progression of keratoconus.
When it comes to correcting vision, in the early stages of keratoconus, eyeglasses or soft contact lenses may be sufficient. As the condition progresses, specialty contact lenses can help provide better visual acuity by creating a smooth optical surface. For individuals with more advanced keratoconus or those seeking better vision in glasses, surgical interventions such as Cornea Tissue Addition Keratoplasty (CTAK), topography guided PRK, intracorneal ring segments or femtosecond laser guided corneal transplantation may be recommended to stabilize the cornea and improve vision.
Managing Keratoconus: Tips for Everyday Life
Living with keratoconus may present challenges, but there are steps you can take to manage the condition and maintain good eye health. Avoid rubbing your eyes, as this can exacerbate corneal thinning. Protect your eyes from excessive UV exposure by wearing sunglasses with UV protection. Follow a healthy diet rich in antioxidants and vitamins to support overall eye health. Regularly visit your eye care specialist for comprehensive eye examinations to monitor the progression of keratoconus and adjust your treatment plan accordingly.
Keratoconus vs Astigmatism: What’s the Difference?
Keratoconus is a disease process which results in irregular astigmatism. Astigmatism is a condition that affects the shape of the cornea and can cause visual disturbance. The key is to diagnose whether a patient has regular or irregular astigmatism. Regular astigmatism is a refractive error characterized by an oval shaped cornea or lens, leading to blurred vision at all distances which is correctable with glasses or soft toric contact lenses. Keratoconus, on the other hand, involves progressive thinning and bulging of the cornea, resulting in irregular astigmatism and a distorted and blurred vision which is frequently not correctable with glasses or standard soft toric contact lenses. In fact, keratoconus is often misdiagnosed as a regular astigmatism in its early stages. While regular astigmatism can often be corrected with glasses, contact lenses, or LASIK surgery, keratoconus may require specialized treatment options such as rigid gas-permeable contact lenses or surgical interventions.
Finding a Keratoconus Specialist
When seeking treatment for keratoconus, it is essential to find a qualified and experienced eye care specialist who specializes in the management of this condition. The CLEI Center for Keratoconus was formed in 2002 as the first dedicated subspecialty center for keratoconus in the US. Our devotion to keratoconus patients is manifest in our advanced diagnostic instruments, our custom specialty contact lenses, and our highly advanced surgical techniques. We work diligently to provide customized and comprehensive treatment plans for each of our patients with the goal of preventing disease progression and optimizing your vision.
Our world renowned center is led by Dr. Steven Greenstein and Dr. John Gelles, who have been at the forefront of clinical research on keratoconus for decades. We took the lead in the pivotal FDA trial that led to the approval of corneal crosslinking, and we continue to innovate and improve upon corneal surgical techniques and specialty contact lenses for keratoconus. Our experience, skill, expertise, and devotion to continuing research is unparalleled. If you are looking for keratoconus care of the highest quality, schedule an appointment with us today.
Conclusion: Empowering Individuals with Keratoconus
Keratoconus is a complex eye condition that can significantly impact vision and quality of life. By understanding the causes, symptoms, and diagnosis of keratoconus, individuals can take proactive steps to manage the condition effectively.
With the support of CLEI’s qualified eye care specialists, you can achieve improved vision and lead a fulfilling life. Remember to prioritize regular eye examinations, follow your treatment plan, and seek support from your eye doctor to navigate the challenges of living with keratoconus.
Again, if you suspect you may have keratoconus or have been diagnosed with the condition, feel free to schedule an appointment at the CLEI Center for Keratoconus today. Don’t let keratoconus limit your vision and quality of life – take control of your eye health today.




