Corneal Tissue Addition Keratoplasty (CTAK) is a novel tissue addition technique that improves corneal curvature and vision for patients with keratoconus. Keratoconus is characterized by thinning of the cornea resulting in a steep cone shape and irregular astigmatism. In technical terms, CTAK is a form of lamellar keratoplasty where a customized sterilized corneal stromal inlay is shaped by a femtosecond laser, then inserted into a corneal stromal channel, also created by a femtosecond laser.
CTAK can improve visual acuity, corneal topography, and quality of life, offering hope to individuals with keratoconus who have been told their only surgical option is a corneal transplant. How exactly does the procedure work and what are the benefits? Let’s dive into the specifics.
Corneal Tissue Addition: A Brief History
CTAK was invented at the Cornea and Laser Eye Institute. Our doctors developed the procedure using patient specific, laser-cut corneal tissue to address the visual and structural abnormalities caused by keratoconus. The first clinical trials began at the Cornea and Laser Eye Institute in 2016. More recently, the outstanding CTAK results were featured on the cover of the Journal of Cataract and Refractive Surgery in July of 2023. CTAK has been established to be safe, effective, and one of the most exciting procedures developed for managing keratoconus.
Who is Corneal Tissue Addition For?
CTAK was developed with keratoconus patients in mind. Keratoconus is a progressive disease that comes from a focal corneal thinning. Over time, the thinner, weaker part of the cornea loses biomechanical strength, which causes the cornea to steepen and bulge. A normal cornea is shaped like a symmetrical dome, but a keratoconus patient’s cornea becomes asymmetrical and cone shaped. This in turn causes distorted optics and vision. Patients often experience visual disturbances such as halos, glare, flares, smears, overlapping images, multiple images, streaking, and starbursts. Currently, there is no cure for keratoconus, which is why disease management is so important.
Typically, keratoconus management can be divided into three parts known as KC 1…2…3:
- Stabilization – Specialty Corneal crosslinking or standard crosslinking can be performed to halt the progression of keratoconus and preserve existing vision.
- Improvement of corneal shape – Intacs, topography-guided PRK, conductive keratoplasty (CK), or CTAK can all help to improve corneal topography, with CTAK offering some unique benefits for patients that qualify.
- Correction of prescription – Glasses, specialty contact lenses, PRK, or ICLs can help refine a patient’s vision further.
CTAK is particularly beneficial for keratoconus patients thanks to the customized tissue inlay utilized during the procedure. For other keratoconus procedures, the cornea needs to be an appropriate thickness, and steepening must be in a treatable area and range. With CTAK, the customized inlay allows us to treat thinner corneas, and to fit the inlay around most cones, which makes treating very steep corneas possible. It also allows us to modulate the amount of flattening we want to induce.
Where Does the Tissue Come From?
The tissue used in CTAK is harvested from a donor after meeting all criteria of the Eye Bank Association of America (CorneaGen, USA), frozen to inactivate the cells, then sterilized with gamma irradiation. This decreases the chance of any bacterial or fungal components that can be associated with corneal tissue as well as inflammatory response. The sterilization process eliminates the donor cells leaving only the collagen lamellae of the cornea for implantation. Over time, the patient’s cornea cells have been shown to repopulate this tissue, making rejection of these inlays very unlikely. Once sterilized, the preserved corneal tissue is then cut into a customized shape before being inserted into the patient’s eye.
Corneal Tissue Addition Vs. Corneal Transplants
One of the most common questions we receive about CTAK is, “Is this procedure the same as a corneal transplant?” To answer that question, consider what happens in a traditional corneal transplant. During a corneal transplant, diseased corneal tissue is removed from the patient’s eye and replaced with fresh (non sterilized) donated corneal tissue. There is more than one kind of corneal transplant. A full thickness corneal transplant (penetrating keratoplasty) involves removing the entirety of the cornea in a specific location from the top to bottom and replacing that area of the cornea with donor tissue. More recently, we can replace specific layers of the cornea – perhaps just the top areas or just the bottom areas of the cornea – which allows us to replace much less tissue. In keratoconus, when we replace the top layers of the cornea, it is called a deep anterior lamellar keratoplasty (DALK). CTAK, on the other hand, does not involve replacing corneal tissue, but rather adding preserved corneal tissue to reshape the cornea.
Penetrating keratoplasty or deep anterior lamellar keratoplasty may be necessary in advanced cases of keratoconus, especially when dense central scarring is present. However, in many cases, CTAK is a less invasive alternative that can provide significant improvements in corneal topography and visual acuity without some of the potential complications associated with a full thickness or partial thickness transplant. For example, since CTAK tissue is gamma-irradiated, the risk of rejection is reduced compared to a full corneal transplant. The recovery period is much shorter too.
What Happens During the CTAK Procedure?
Before Surgery
First, we use multiple devices to map the cornea. With this information, we create an exact model of the curvature and elevation of cornea. We also determine the location and size of the cone. Then, a surgical plan (using software designed at the Cornea and Laser Eye Institute) is carefully designed to provide optimal tissue placement. We prepare the preserved tissue according to the surgical plan, which allows us to give patients customized corrections for the most effective treatment.
How exactly is the tissue prepared? A femtosecond laser is used to cut the tissue, shaping it to fit each patient’s specific needs. This is the same laser used to create corneal flaps in LASIK surgery. It is ultra precise, and can create just the right width, diameter, length, and angle needed for a custom tissue inlay, based on the results of an individual corneal map.
Just before CTAK, we prepare patients with numbing drops so they are comfortable throughout the duration of the procedure.
During Surgery
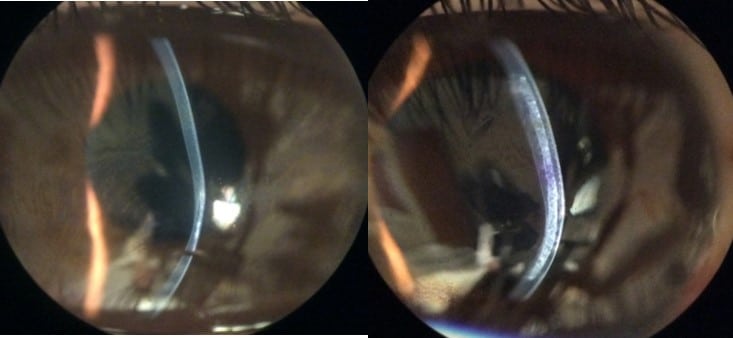
During surgery, we use the femtosecond laser to create a channel in the cornea where the inlay will be inserted. By using a femtosecond laser to shape the inlay and to create the channel, we can ensure that the size and shape of the channel matches the size and shape of the inlay with complete precision.
Next, we use surgical tools to insert the corneal tissue inlay into the channel, which adds thickness to the cornea and decreases the irregularity and cone shape. The entire procedure takes less than 30 minutes.
After Surgery
Patients are given a corticosteroid drop after the procedure to prevent inflammation, and antibiotics to prevent infection. After CTAK, most patients will notice an improvement of vision in the first week after surgery. It is important to remember that while CTAK improved uncorrected vision, in most cases it is used to improve vision in glasses and contact lenses. Your glasses and contact lens prescription will be checked starting around one month after surgery. Follow up appointments will be required to make sure your eye is healing properly and adapting to the tissue addition.
CTAK Risks
As with any surgical procedure, not everyone is a candidate and there are some potential risks. Infection is a normal risk associated with surgery, and CTAK is no exception. Patients receive antibiotics post-operatively, so the risk is small but it exists. Inflammation or scarring is another risk factor, which is why patients receive a corticosteroid drop after the procedure is complete. A third risk is unexpected or worsened corneal shape. While it is an unlikely outcome, it can be reversed simply by removing the corneal tissue addition. This is another big benefit of CTAK: it is completely reversible. In fact, if the first CTAK results in an unfavorable outcome, it may be possible to reshape the tissue addition and perform CTAK a second time to achieve the desired outcome.
Corneal Tissue Addition Outcomes
One of the benefits of CTAK is the significant improvement of a patient’s vision. Consider some results from the clinical trials we began conducting in 2016.
On average, patients saw:
- uncorrected vision (without glasses) improved by about 5 logMAR lines (from 1.21 logMAR lines (20/327) to 0.61 logMAR lines (20/82)).
- vision in glasses improved by over 3 logMAR lines (from 0.62 logMAR lines (20/82) to 0.34 logMAR lines (20/43))
- and glasses prescriptions improved (from -6.25 diopters to -1.61 diopters).
CTAK also improves corneal topography. The topographic analysis in the same clinical trial showed a significant flattening of the cornea, with an average decrease of -8.4 D in Kmean and -6.9D in Kmax at 6 months after the procedure.
Conclusion
CTAK represents a significant advancement in the treatment of keratoconus. With the ability to effectively improve visual acuity, corneal topography, and patient quality of life, it is a promising option that is less invasive and more personalized for individuals with this challenging eye condition. If you’ve been told that corneal transplant is your only surgical option, contact us today to find out if CTAK could be an appropriate alternative.



