Located: Corner & Laser Eye Institute 300 Frank W
Burr Blvd, Teaneck, NJ 07666, United States
201-692-9434
The CLEI Center for Keratoconus was founded in New Jersey in 2002 as a subspecialty division of the Cornea and Laser Eye Institute. It is the first dedicated subspecialty center for keratoconus in the nation. The New Jersey Center led today by Dr. Steven Greenstein and Dr. John Gelles is world-renowned, leading the FDA pivotal trial for the approval of corneal crosslinking, innovating and improving upon corneal surgical techniques, and developing unique specialty contact lenses for keratoconus.
In the CLEI Center for Keratoconus, we are devoted to all aspects of keratoconus. From our advanced diagnostic instruments, to our customized specialty contact lenses, and to the most advanced surgical techniques we are committed to always providing the most comprehensive and state-of-the-art keratoconus care.
Communication among providers is particularly important in keratoconus, and our doctors and staff work collaboratively to provide patients with customized and comprehensive treatment plans to prevent disease progression and optimize your vision.
When you decide to trust your vision to our team, we are committed to taking care of all your keratoconus needs. From the beginning to the end of your keratoconus journey, you will be treated by our highly experienced team of keratoconus specialists. At CLEI, we pride ourselves on taking the time to explain your treatment options and answer all of your questions at every visit. We understand everyone has unique circumstances and we take the time to understand your individual visual needs.
Most of our cornea and laser procedures are performed in-office, ensuring that your procedure will be performed in a familiar environment with our experienced team; reducing stress on your surgery day. Our lens-based and corneal transplant procedures are performed in a local state of the art surgical center dedicated solely to eye surgery.
At CLEI, keratoconus patients undergo a comprehensive examination using all of the latest technology. With our KC 1,2,3 approach, your individual needs are matched to a customized treatment plan to, one… stabilize your cornea, two…improve your corneal shape, and three… correct your long-term vision.
We offer cutting edge surgical treatment including unique approaches to corneal crosslinking, topography guided PRK, CTAK corneal inlays, Intacs, and femtosecond laser guided corneal transplants, to stabilize your cornea and improve your corneal shape.
To correct your vision, we offer the most modern specialty contact lenses, including customized soft lenses, scan or impression based scleral lenses, with further visual clarity from individualized higher order aberration correction. Vision correction with PRK, EVO ICL, RLE, or cataract surgery may also be possible in certain cases. While not every patient will need all of these treatments to be performed, it is critical to be evaluated and treated by doctors who perform all of these procedures to ensure that an optimal treatment plan is designed for you.
In addition to clinical care, the CLEI Center for Keratoconus is at the forefront of clinical research. We are not just doctors, we are academicians and researchers who continue to be at the cutting edge of keratoconus diagnostics and treatment. We have published many of the most cited manuscripts in the literature; and perform many of the most rigorous clinical trials in the field. Our doctors have delivered thousands of academic lectures, published hundreds of peer-reviewed manuscripts, authored numerous academic book chapters, led multiple FDA clinical trials, written several books, and hold multiple granted patents derived from our research. Our experience, skill, and expertise are simply unmatched. To get a full understanding of our expertise please review our compendium of work here.
Understanding Vision from Normal Corneas versus Keratoconus and Irregular Corneas
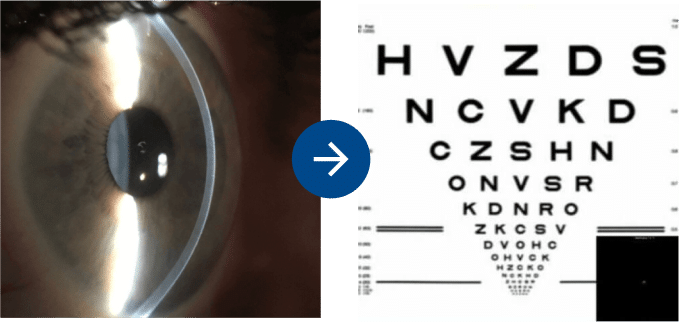
Profile of a normal cornea, note the smooth dome shape.
Vision Simulation of a healthy eye with a normal cornea wearing glasses.
The eye is similar to a camera. In the eye, the cornea and the internal lens help light focus on the retina. The cornea is analogous to the front lens on a camera. Normal corneas have a smooth dome shape, which allows light to focus to a single, sharp focal point. In a perfect eye this focal point lands on the retina. If the focal point is in front of or behind the retina the vision is blurry. This misalignment is called refractive error. Glasses, contact lenses, or vision correction surgery can aid in moving the focal point to the retina, thereby creating clear distortion-free vision.
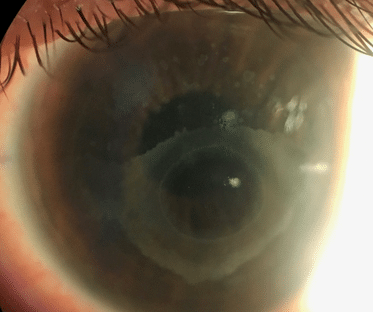
Profile of a keratoconus cornea. Note the peaked shape and focal thin region.
Vision simulation from an eye with keratoconus wearing glasses.
Keratoconus is a disease which manifests with an irregular corneal shape. The cornea becomes steeper resulting in a conical rather than a dome shape. This conical shape causes light to distort, resulting in multiple focal points on the retina. Many patients will describe their blurred vision as distorted, overlapping, or ghosted. Frequently, these irregularities are also responsible for glare, flare, and halos around lights. Glasses and standard soft contact may help in moving the multiple focal points back toward the retina, but these focal points remain separate and frequently the vision remains distorted. These remaining visual distortions are referred to as higher order aberrations.
We understand that keratoconus is more than a disease, it affects everything about your life. Every waking moment can be a reminder of your Keratoconus eye disease. Our goal is to improve the quality of life for those affected by keratoconus. To do this we take a comprehensive approach to your treatment which we call KC 1, 2, 3.
Since we started treating patients, as part of the initial clinical studies in the US, with crosslinking in 2008, crosslinking has emerged as one of the most important advancements in keratoconus treatment. Corneal crosslinking (CXL) halts the progression of keratoconus to preserve your vision and prevent worsening of disease. Corneal crosslinking makes the cornea stiffer and more resistant to disease progression over time.
In this procedure, riboflavin (Vitamin B2) is administered in conjunction with ultraviolet A (UVA – 365nm) light. The interaction of riboflavin and UV light causes a photobiologic reaction in the cornea leading to the formation of additional molecular bonds between collagen molecules and their supporting biological sugars. This results in the stiffening of the cornea, much like placing additional cables on a bridge will help to support the bridge structure. At our center, we offer standard and specialty crosslinking options.
Standard crosslinking was FDA approved in 2016. This is the original crosslinking procedure applying traditional riboflavin formulations (dextran mixed and saline mixed) with constant ultraviolet light exposure.
Our center was the medical monitor and played a central role in the pivotal U.S. Multicenter Clinical Trial of Corneal Collagen Crosslinking leading to the FDA approval. Dr. Peter Hersh was the lead author of the two studies leading to approval and Dr. Steven Greenstein wrote many of the seminal papers about crosslinking in the US.
What to Expect after Standard Crosslinking?
The first phase of healing is the early period (1 to 5 days) when the surface epithelial cells heal. Generally, a bandage contact lens will protect the cornea and make it comfortable during this time.
There may be some discomfort, primarily on the first day, when the procedure is done. You will be able to see through the bandage lens, but vision will be hazy during this time (like driving with a foggy windshield). In some patients, vision may continue to be mildly hazy for several months, but, in general, nearly all patients note a return to their baseline vision over the first few weeks.
Contact lens wear can be restarted after we are satisfied with the early healing, usually around 2 weeks to 1 month after the procedure. Remember, crosslinking is designed to decrease the progression of keratoconus and corneal ectasia. It is not expected to improve your vision. Other procedures can be performed to further improve your vision.
It is important to know that, although crosslinking will successfully stabilize disease progression in most patients, in rare cases keratoconus may continue to progress. It is extremely important that you continue to be monitored on a regular basis after CXL is performed.
Since the original studies of corneal crosslinking, there have been modifications to the standard crosslinking technique. These include modifications to the UV light, such as power and time of exposure, and riboflavin formulations. In addition CXL can be performed in conjunction with other corneal reshaping procedures to further improve results.
This version of the crosslinking procedure-has one modification; you may be treated with an isotonic riboflavin solution. This new riboflavin solution (mixed with hydroxymethylcellulose, HPMC) may limit the dehydration (thinning) of the cornea, frequently seen during the standard CXL procedure. By limiting corneal thinning during the CXL procedure, the cornea can be treated in its more natural state. This may allow more patients to be treated with CXL and reduce the need for additional procedure time to place hypotonic riboflavin during the CXL procedure. In the standard CXL procedure, if a cornea becomes too thin with the dextran mixed riboflavin, the UV light portion of the procedure is delayed until the saline mixed riboflavin can swell the cornea to a sufficient thickness to proceed. Rarely if the cornea cannot be adequately swollen the procedure may need to be canceled.
This study aims to evaluate the efficacy of isotonic riboflavin solution for crosslinking. The second goal of this study is to determine whether there are any significant outcome differences between administering isotonic riboflavin with HPMC and standard riboflavin with dextran.
Transepithelial crosslinking is sometimes called the “epi-on” CXL technique. In transepithelial crosslinking, the epithelium (the surface layer of the cornea) is not removed. The epithelium of the cornea is similar to your skin. It is a barrier for the riboflavin and UV light to enter the corneal stroma which is critical for effective crosslinking to occur. Modifications to the standard crosslinking procedure, including new riboflavin solutions which penetrate through the epithelium, higher power UV light irradiation, and additional oxygenation of the cornea during UV light treatment, are being performed to improve the efficacy of the epi on procedure.
It has been proposed that epi on CXL offers several advantages over standard crosslinking. Since the epithelial barrier is not broken, there may be a reduced risk of infection, thereby increasing the safety profile of this procedure. Additionally, there may be a faster visual recovery and improved patient comfort in the early postoperative healing period since re-epithelialization of the cornea is not required.
Currently, there are no FDA approved transepithelial crosslinking procedures in the US. This study compares two variants of transepithelial crosslinking. During the UV light treatment, some patients will be treated with a riboflavin drop every 2 minutes, and others will be treated with a riboflavin drop every 10 minutes. The primary goal of this study is to evaluate the efficacy of epi on CXL in these two groups. The secondary goal of this study is to determine if there is equivalency between groups.
This study is being conducted to determine the efficacy of accelerated corneal crosslinking. In this case, accelerated means that the power of the ultraviolet light is higher than in the standard procedure, therefore it can be administered over a shorter period of time so the total UV treatment dose remains the same.
There are two randomly assigned groups in this study, however both groups will receive accelerated crosslinking treatment. All patients will have the corneal epithelium removed, similar to the standard CXL procedure. One group will be treated with 12mW/cm2 of continuous UVA light treatment for 7.5 minutes and the other group will be treated with 12mW/cm2 of pulsed (1 minute on, 1 minute off) UVA light treatment for 15 minutes. The total power of UV light in these two groups is the same.
This study aims to evaluate the safety and efficacy of accelerated corneal collagen crosslinking treatments performed with either continuous or pulsed (on-off) UVA light for reducing corneal curvature. Secondarily, this study aims to determine if there is equivalency between groups.
This study aims to evaluate the safety and efficacy of a new UV light source and riboflavin formulation. The NXL System uses laser diodes instead of the broad beam used by all other UV systems. This allows for precise patterns of UV light to be projected on the cornea, and with the pulsation of the UV, there is time for reoxygenation of the cornea during the procedure as well. The epithelium is not removed for this procedure making this an alternative “epi on” technique.
Using the excimer laser, a topography guided treatment is performed to selectively apply laser to the steepest portion of the cornea, thereby removing the epithelium, and a small amount of stroma, primarily over the keratoconus cone. Riboflavin is then applied to hypersaturate the exposed cone region. The resulting crosslinking is more focused in the biomechanically weak region over the cone, consequently strengthening this area more effectively. Since only a small portion of the epithelium is removed healing may be much quicker than traditional crosslinking.
At the CLEI Center for Keratoconus we are constantly staying at the forefront of CXL treatment and our list of available clinical trials is expanding. To learn more about which crosslinking option is recommended for you, schedule an evaluation with one of our keratoconus specialists near you today.
Keratoconus causes a corneal shape deformation, which results in distortion of vision. Vision can be improved by undergoing certain procedures designed to improve corneal shape. This is a critical part of comprehensive keratoconus management. Improvement in corneal shape will allow you to have a better quality of vision in glasses and soft contact lenses and in certain cases may improve uncorrected vision as well. Although every patient with keratoconus will not require a corneal reshaping procedure, it is important to be evaluated at a center performing all of these procedures to learn whether you may benefit from any of them. Our CLEI doctors are experts and innovators and will select the correct corneal reshaping treatment to optimize your cornea and vision.
This procedure was invented at CLEI, and our first clinical trials for the CTAK procedure began in 2016. CTAK has proven safe, effective, and one of the most exciting procedures developed for keratoconus management. It uses a custom-shaped segment of irradiated corneal tissue, placed in a channel created by the femtosecond laser, which induces reshaping of the cornea and improved vision. Read more about CTAK here.
Our center has extensive experience with Intacs. We performed and published on some of the largest clinical trials related to Intacs for keratoconus with generally good results. Today, we are typically performing more customizable procedures such as CTAK and TG-PRK in many of our keratoconus patients who would have been Intacs candidates in the past. However, Intacs may still be beneficial in some cases.
Schedule a full evaluation with one of our keratoconus experts to determine which procedure may be right for you.
Intacs are implantable intracorneal ring segments (ICRS). Intacs are made of polymethylmethacrylate (PMMA), an inert polymer used in eye surgery for many years. They were originally FDA-approved in 1998 for nearsightedness and later received approval for the treatment of keratoconus. The goal of Intacs is to reshape the cornea in keratoconus. The thickness and position of the Intacs segments are chosen based on your individual corneal shape. Depending on the individual measurements, one or two segments may be placed in the cornea.
In some cases, Intacs may need to be removed for certain medical complications such as infection or persistent corneal inflammation. Previously, some Intacs segments were removed for poor visual results. Now many of these patients benefit from TG-PRK to further improve corneal shape and vision without removal of the Intacs segments. In other cases, Intacs can be removed and a CTAK procedure can be performed with better visual results. If you had Intacs placed in the past, contact the CLEI center for keratoconus to schedule an in depth keratoconus exam and see if you are a candidate for further improvement with one of our other keratoconus procedures.
At the CLEI Center for Keratoconus, we offer all types for cornea transplants, including full-thickness transplants called a penetrating keratoplasty (PK), partial-thickness transplants, also called deep anterior lamellar keratoplasty (DALK), and laser-assisted procedures. We prefer the newer femtosecond laser-assisted procedures for many of our keratoconus patients.
With subspecialty fellowship training in corneal surgery and years of transplantation experience, the CLEI team works to provide you with the best possible option for your surgery and visual outcome. The overall success rate of a corneal transplant is very high when using modern eye banking and surgical techniques. For instance, keratoconus has one of the best prognosis for good vision, with a greater than 90% chance of a clear graft. However, many factors can influence the outcome. After surgery, the transplant must be monitored for signs of graft rejection. In most cases, vision gradually returns after surgery.
Patients must remember that the healing process may vary greatly from one individual to another. Some patients may experience improved vision within a few weeks after surgery, while for others, it may take up to a year. Glasses or contact lenses are still necessary after most corneal transplants, and a variety of vision correction procedures may be useful after transplantation.
The procedure usually takes approximately one hour and is performed with either general or local anesthesia on an outpatient basis. If you are having a laser-assisted procedure, the laser portion of your surgery will take place at CLEI, and then you will be transported to our outpatient surgery center.
After the surgery, you will go home with your eye covered by a patch and a plastic shield to protect the eye. When you see us the day after surgery, we will start your medicated eye drops. You may use drops for a year after surgery to prevent rejection of the transplant, and stitches may remain in the cornea for several years in some cases.
In keratoconus, maximizing vision has the greatest impact on your quality of life. This can be achieved both surgical and non-surgically.
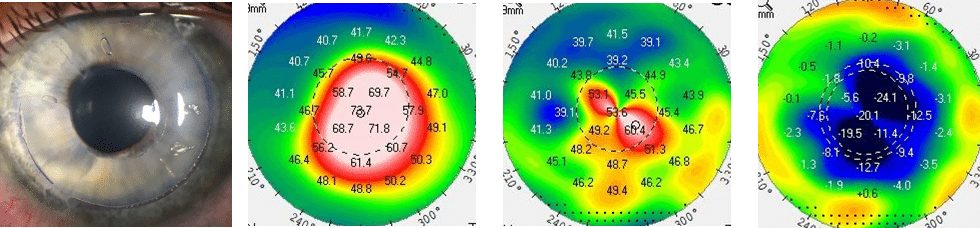
The process of designing a customized lens to meet the needs of keratoconus patients starts with an advanced and in-depth evaluation. This evaluation guides the process of understanding which type of specialty contact lens will meet your individual needs. A multitude of different scans, impressions, and diagnostic lenses may be used in the design process. Once a lens type has been selected, our keratoconus contact lens specialists will create a custom contact lens for you.
Our keratoconus doctors work extensively with all contact lens designs and have helped suffering patients from all over the world. Many patients who have been told that they can not be fit with a scleral lens and require corneal transplantation have been successfully fit by our contact lens experts with a custom designed scleral lens. Here at the Cornea and Laser Eye Institute, we have been instrumental in developing advanced technology, fitting techniques and different lens designs. As experts and developers of many of these techniques, our doctors will determine which approach will be best to create a custom lens or device to meet your individual needs. This process generally involves several revisions or modifications to ensure the lens is ideally fit, your eye health is maintained, and your vision is the best possible.
Most patients are familiar with standard soft lenses. These lenses are mass-manufactured in a process called cast molding. The lens parameters are generally limited to fit the average shape, size, and power needs of a normal eye. Though they are highly successful for most individuals with uncomplicated corneas and average refractive errors, those patients with moderate to advanced corneal irregularity commonly experience difficulty with these commercially available lenses. However, in certain cases, our CLEI contact lens experts are able to fit individuals with mild corneal irregularity and refractive error in standard soft lenses with a satisfactory outcome.
Unlike their mass-produced counterparts, custom soft lenses are not limited to the typical parameter constraints of the normal corneal population. Custom soft lenses are lathe-cut and can be produced in an extensive range of base curve radii, diameters, materials, and nearly endless refractive powers. Some of these lenses can have a cosmetic or prosthetic option added, which can be useful to improve cosmesis and to reduce glare. Additionally, lens thickness can be significantly increased to create a pseudo-rigidity, which can mask corneal irregularity. Success of these lenses depends on the severity of your corneal irregularity. For individuals who are unable to tolerate corneal GP lenses, custom soft lenses may provide adequate vision and improved levels of comfort. At the Cornea and Laser Eye Institute, our doctors have been able to fit custom soft contact lenses for many patients who were told that rigid lenses were their only contact lens option.
Corneal GP lenses are the classic choice to mask corneal surface irregularities and to improve visual acuity. These lenses are also referred to as hard lenses, rigid lenses, and RGP (rigid gas permeable) lenses. Using corneal GP lenses on a cornea that has very minor irregularity is similar to fitting them for refractive correction on a normal cornea. These lenses are lathe-cut and can be produced in an extensive range of base curve radii, diameters, materials, and nearly endless refractive powers.
When fitting a corneal GP lens, precision of fit is of the utmost importance to maintain the corneal integrity and lens comfort. However, fitting corneal GPs becomes increasingly difficult as the corneal surface becomes more irregular. Success of these lenses depends greatly on the severity and location of the corneal irregularity. Many patients who have had difficulty with GP lenses in the past generally have irregularity that is too severe to be successful with this lens design.. At the Cornea and Laser Eye Institute our contact lens specialists fit a wide variety of specialty contact lens designs to ensure that the right contact lens design will be used for your specific eye condition.
For patients experiencing reduced comfort or minor epitheliopathy (damage to the surface layer of the cornea) with a best-fit corneal GP, a piggyback lens system can be utilized. This approach uses a GP lens to improve visual acuity, while the underlying soft lens provides corneal protection, cushioning the cornea from the GP lens and improving comfort. The piggyback lens system may be best utilized when other options have failed and the RGP lens remains the best option for vision correction.
Patients may be apprehensive to adopt this modality due to the perceived difficulty of wearing and caring for two lenses. Frequently, daily disposable standard soft lenses can be used as the soft lens in the piggyback system to simplify care. On occasion a custom soft lens option, such as a cosmetic/prosthetic soft lens or a soft lens with a central excavation (allowing the GP lens to rest in a depression in the soft lens surface), is required to improve cosmesis, reduce glare, or improve lens centration.
Hybrid lenses utilize a GP center with a soft lens edge, so they have characteristics of both GP and soft lenses. Various hybrid lens designs exist, with multiple geometries to accommodate a mild to moderate corneal irregularity. The GP portion of the lens can be modified to align with or vault over the corneal irregularity while the soft skirt aids in adjusting lens movement, tear exchange, and lens centration and can also influence alignment of the GP portion of the lens. Hybrids can produce improved vision and comfort over corneal GPs in cases of lens decentration and lens intolerance. Of note, quality of life is similar with corneal GP, soft, and hybrid lenses. Hybrid lenses are filled with saline prior to lens application and because of the soft edge special attention to the force of lens application is required to avoid issues with lens wear.
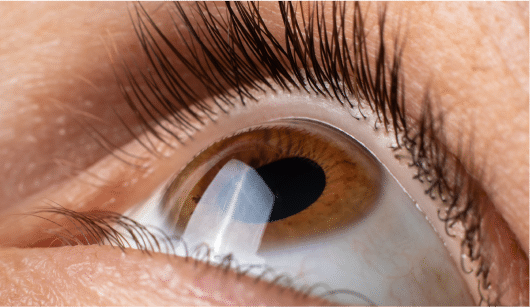
When corneal irregularity is advanced, scleral lenses are preferred over other lens designs. These lenses vault over the cornea, aligning with the sclera and overlying conjunctiva (white of the eye). Scleral lenses can overcome nearly any corneal irregularity and should be considered as an option prior to referral for corneal transplantation. Individuals who have keratoconus and who otherwise would have undergone corneal transplantation secondary to contact lens failure can achieve success with these lenses.
These lenses are designed with a myriad of unique modifications. These lenses are lathe-cut and can be produced in an extensive range of shapes, diameters, materials, and nearly endless refractive powers. Properly fitting scleral lenses should fit comfortably with adequate vision correction. Custom scleral lenses are designed by using a diagnostic scleral lens set. A series of lenses with varying shapes are placed on the eye. The lens fit is evaluated, and during the design process, modifications to the lenses are made based on observations and eye performance. At the Cornea and Laser Eye Institute, our doctors have over 100 different diagnostic contact lens sets at their disposal. In contrast, the average practitioner may have 1 or 2 diagnostic sets.
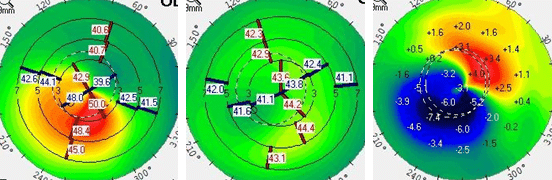
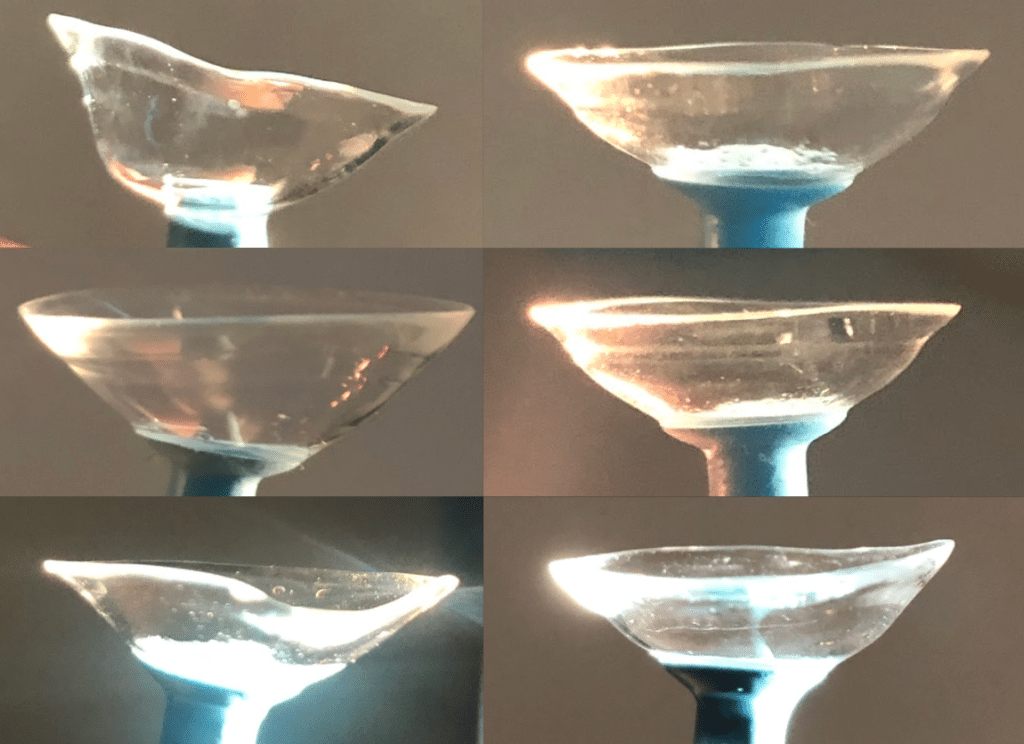
Occasionally custom scleral lenses will be unsuccessful due design limitation or due to the complex shape of the eye. In those cases even more advanced scleral lenses and prosthetic scleral devices can be used. The use of advanced computer aided design softwares and advanced fitting techniques such as impression based and scan based design, may be utilized to achieve a healthier and more comfortable contact lens fit. In addition, highly customizable optics such as wavefront guided, higher order aberration correcting optics can be added to some lenses for improved visual correction.
Our doctor works extensively with these devices and has helped suffering patients from all over the world. He has been instrumental in developing advanced technology, fitting techniques and lens designs. Custom made scleral lenses, whether derived from diagnostic fitting, software driven, scan based or impression based data, all can lead to a successful result. As an expert in these techniques, our doctor determines which approach will be best so he can create a custom scleral lens or device to meet your individual needs.

A custom scleral lens made by a scan or impression based design technique. Notice the unique shape of the lens, designed to fit the exact nuances of the cornea or ocular surface. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
A variety of custom made scleral lenses, each is made to mimic the ocular shape of the patient’s eye. Note no 2 lenses are the same just as no 2 eyes are the same. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved
The classic way to fit and design scleral lenses is by use of a diagnostic contact lens set. The majority of diagnostic designs have simplified parameter options, which can limit the design options. Scleral lens design software can allow for more design options, allowing for more customized lenses to be made. Several custom scleral lenses or scleral devices, such as a PROSE device, use these powerful software programs allowing our doctors to create more customized lenses.
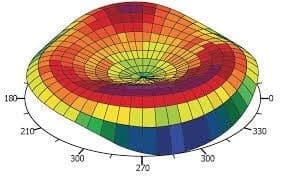
Example of software used to design lenses. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
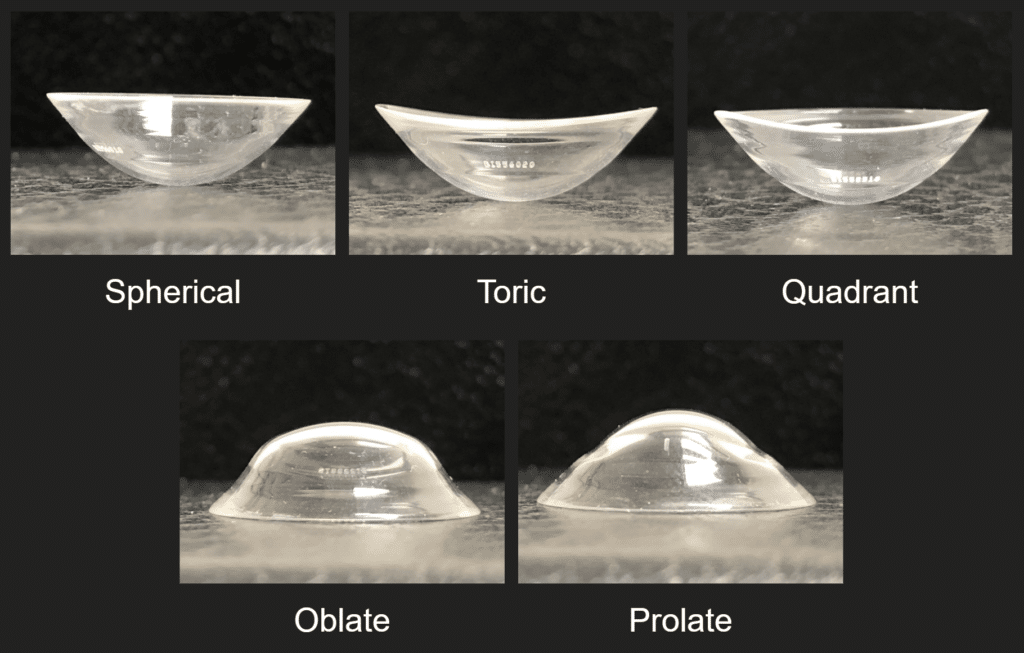
Various derived shapes. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
Another design approach uses highly specialized devices to scan the ocular shape. This shape data is used to create a 3 dimensional digital model of the eye. Once this model is created our doctors will use a specialized computer aided design software to create a lens unique to the contour of the eye. Most doctores, even those specialized in contact lenses, do not have access to these devices, however, at the Cornea and Laser Eye institute we have access to all of the latest devices capable of capturing your scan based data.
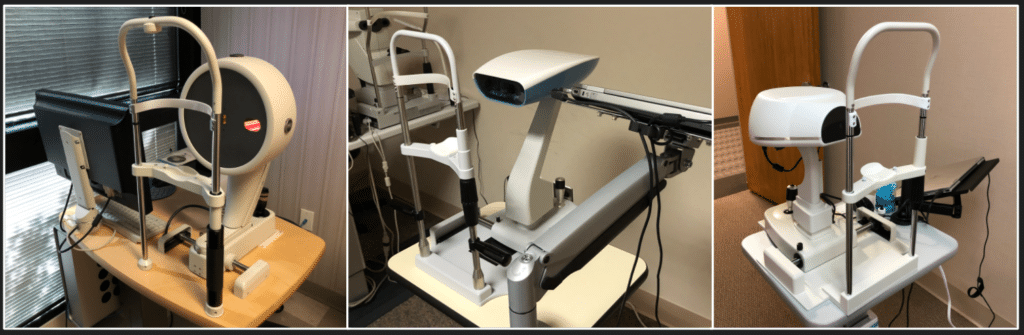
3 different profilometers at CLEI. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
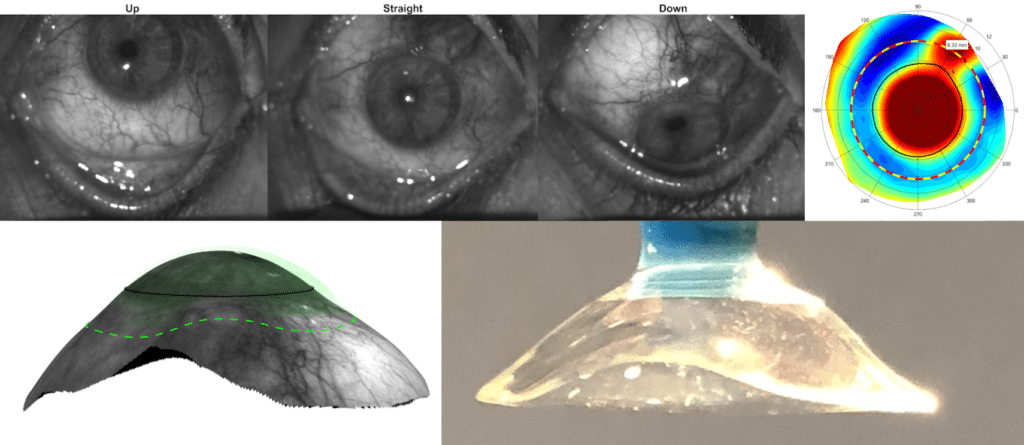
Scans from a profilometer, used to create a 3d model to build a custom scleral lens. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
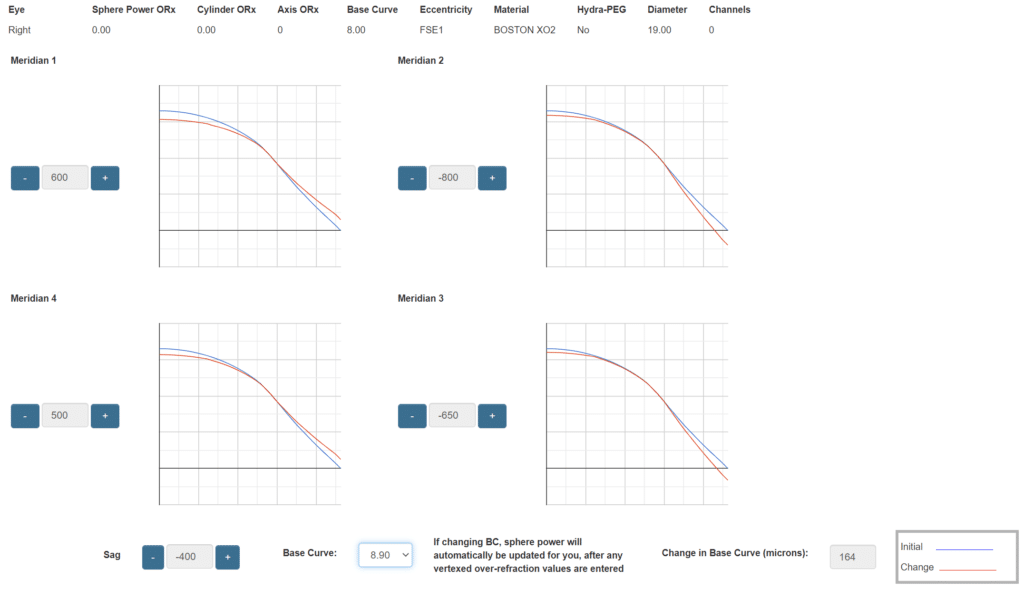
Another approach is the technique of ocular impressions. Using a specialized gel, an impression of the eye is obtained. This impression is the most accurate depiction of your eye possible and is then 3D scanned, creating a digital model of the eye. Using this model and multiple highly specialized computer aided design programs a completely customized scleral lens, such as a EyePrintPro device, can be created.
Our doctors have been pioneers in this technique. The first to perform it in the North East United States and is currently the only doctor trained to do so in the state of New Jersey. Less than 0.1% of practitioners in the world are trained on this technique.

An impression of cornea and ocular surface, this will be 3D scanned and used to create a model of the eye which a custom scleral lens is designed.
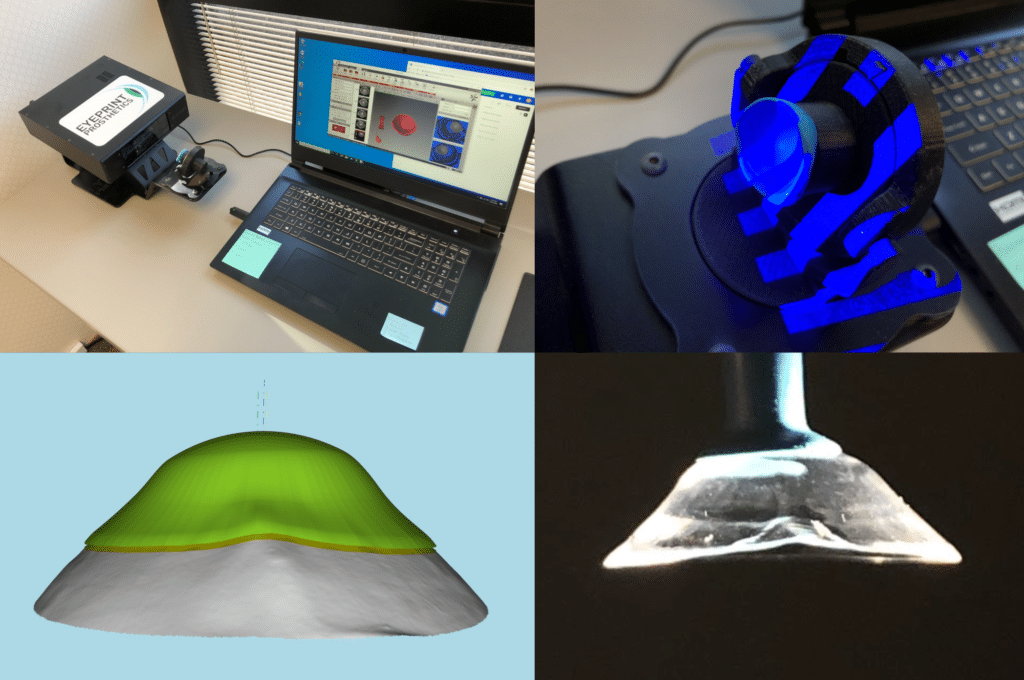
An impression being 3D scanned, a model lens derived, and a custom scleral lens manufactured. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.
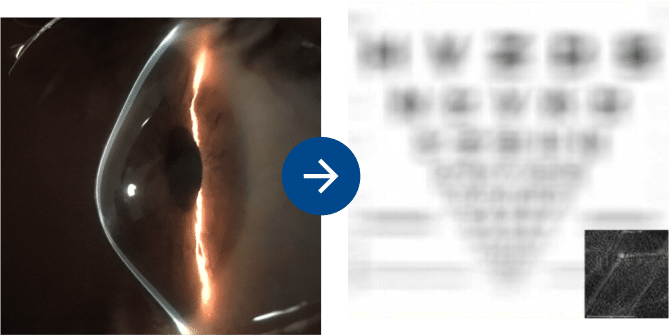
In some cases vision with scleral lenses, though improved, may still have some residual blur. This residual blur is caused by higher-order aberrations. These higher-order aberrations are responsible for doubled, overlapped, ghosted vision with glare, flare, starburst and halos. In these cases, the addition of highly customized wavefront-guided, higher-order aberration-correcting scleral lenses can further improve your vision.
Vision Simulations of Traditional Scleral Lenses & Guided Scleral Lenses
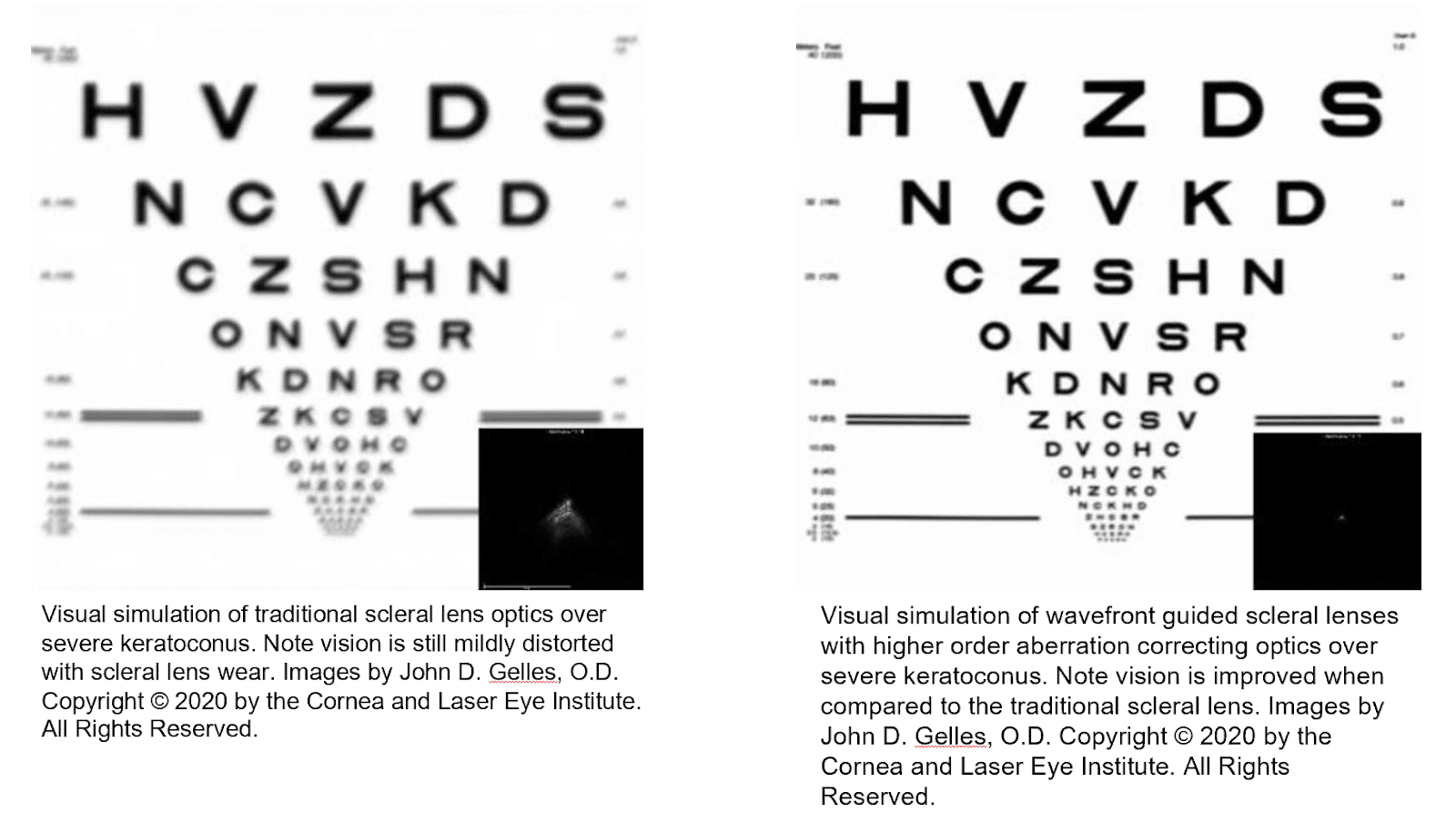
These optics are considered High Definition optics as the clarity is improved over traditional optics. Our doctors were the first to use this technology in the North East United States and are currently the only doctor trained to do so in the state of New Jersey. Our research has found these lenses provide an average 50% percent reduction in aberrations and 1 or more lines of visual acuity improvement over traditional scleral lenses.
In order to fully assess your keratoconus, understand the likely future course of your disease, and make appropriate treatment recommendations, we perform an extensive eye examination with a variety of specialized tests to fully analyze the state of your keratoconus. These tests also give you a complete baseline for your ongoing care in the future.
There are a number of goals of the comprehensive keratoconus evaluation at the CLEI Center for Keratoconus.
First, we want to fully assess and define your keratoconus in order to monitor progression over time. Second, this testing will allow us to best recommend a course of treatment to optimize your visual function.
The CLEI Center for Keratoconus incorporates all of the latest diagnostic technologies to assess your keratoconus and determine the proper course of treatment. Some of these diagnostic tools include:
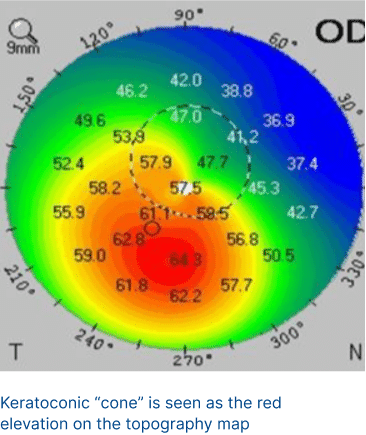
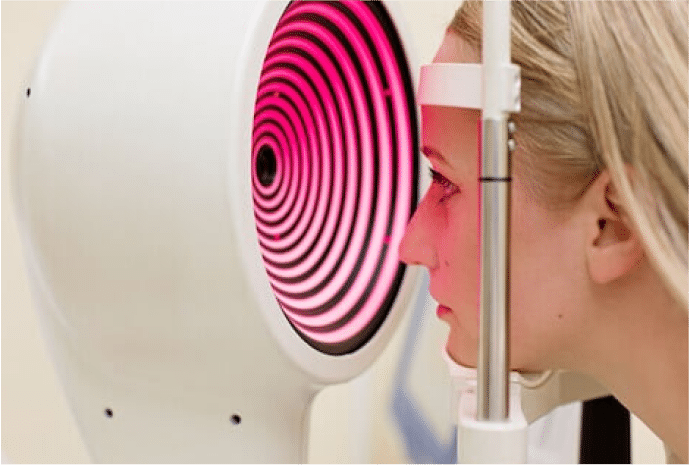
This test that takes a 3D picture of the front part of the eye. It uses a special camera that rotates and captures cross-sections of the cornea. The rotational Scheimpflug camera takes up to 50 cross-sectional images. This helps us see if there are any problems with the thickness or shape of the cornea. The analysis that can be performed in these devices is extremely advanced, allowing us to find keratoconus even before it impacts vision.

This is a test that measures the strength, elasticity and flexibility of the cornea. In keratoconus the corneal strength is reduced leading to stretching and thinning of the cornea. Measuring the corneal biomechanics may allow for better diagnosis of early keratoconus, help to predict its possible progression, and allow for monitoring of changes in the keratoconic cornea. These devices include the Oculus Corvis and Reichert Ocular Response Analyzer.

Keratoconus, one of the more obscure and less widely known eye diseases, occurs in about one out of every 725 individuals and is one of the more difficult eye diseases to diagnose. (More recently in a pediatric study participated in by our Keratoconus doctors the numbers were found to be one out of 344) Keratoconus eye disease is caused by the weakening of the collagen tissue that makes up the cornea. The cornea begins to stretch and thin as the collagen gets weaker, resulting in a loss of the cornea’s normal dome shape.
Biologically and structurally, the cornea is made up of bands of collagen called lamellae which are “glued” together by natural biologic sugars called glycosaminoglycans or GAG’s. The cornea’s collagen and microstructure are abnormal in keratoconus, causing a weakness of the corneal, which then leads to corneal distortion and related visual problems.
It is a progressive condition which, aside from distorting the cornea’s natural optics, can also lead to scarring and other problems. The presentation and impact of keratoconus can vary widely from person to person. In its earliest stages, keratoconus often masquerades as astigmatism or nearsightedness, two of the more common eye conditions. Often, it is only after numerous unsuccessful attempts at vision correction with glasses or soft contact lenses that keratoconus is diagnosed.
Keratoconus is typified by corneal thinning and biomechanical instability. This may be caused by abnormalities in the normal collagen structure of the cornea. Collagen is the main structural component of the cornea. Collagen is a molecule that is typically very strong. For example, it makes up most of the structure of the tendons and ligaments of your muscles and bones. The cornea is made of pancakes (or lamellae) of collagen tissue in a complex array. In keratoconus, the collagen lamellar architecture may be abnormal. There may also be abnormal enzymes that degrade the collagen and reduce the collagen in the keratoconic cornea. In addition, the cells of the cornea (keratocytes) may not be normal, contributing to the thinning and instability of the keratoconic cornea. The linkages of the collagen molecules, collagen lamellae, and corneal sugars to one another may also be weak in keratoconus. For instance, “anchoring fibrils” which normally lock the collagen pancakes to the front of the cornea, on Bowman’s layer, may be abnormal. This may allow the collagen pancakes to slide on one another and exacerbate keratoconus progression. Because of this, it is important that the keratoconus patient does not rub his/her eyes in order to avoid mechanical shearing of the collagen pancakes. Finally, inflammation may also play a role in keratoconus. Reactive oxygen species, or oxygen free radicals, may damage the corneal cells and collagen structure, and lead to keratoconus progression. Because of this, avoiding and treating eye inflammation (for instance, eye allergies) also may be important for the patient with keratoconus.
Detecting keratoconus eye disease can be challenging as its initial symptom is often a minor blurring of vision which can progress to a gradual deterioration in vision that cannot be easily corrected with glasses and standard soft contact lenses. Keratoconus symptoms include:
The actual cause of keratoconus is unclear. It may have a genetic, inheritable component. However, in many patients there are no family members with the disease. Similarly, many children of keratoconus patients do not have keratoconus, but they should be checked in early adolescence for signs of keratoconus because early management can prevent the progression of the condition over time. Keep in mind, the average eye exam does not include tests that are sensitive enough to catch keratoconus so its imperative to see a specialist with the experience and diagnostics necessary to fully assess your child. The CLEI Center for Keratoconus is uniquely skilled
If the last time you learned about genetics was in biology class, you’re not alone. To best understand genetic testing it’s important to revisit the basics. There are two main categories of genetic diseases: Monogenic and Polygenic.
Monogenic disease is simple, if you have the gene you have the disease. It’s a yes or no. A well-known example of this is cystic fibrosis.
Polygenic disease is more complex, no single gene is responsible for the disease, rather, it is a collective of genes associated with a disease. If you have more genes associated with the disease, you have a higher genetic risk of the disease. These genetic factors interact with environmental factors to cause the disease. Keratoconus is a polygenic disease. Other examples of polygenic diseases include hypertension and diabetes.
Genetic tests help to guide personalized, precise, medicine. If a patient is identified with a high genetic risk for keratoconus, then our doctor will prescribe more frequent follow-up, recommend avoiding or treating environmental factors, such as treating ocular allergies and stopping eye rubbing, and may initiate earlier intervention with treatments such as crosslinking. These treatments, if initiated at the earliest onset of the disease can slow the trajectory of the disease, preventing advanced keratoconus.
Both genetic and environmental factors contribute to the development of keratoconus. An example of environmental factors impacting the development of keratoconus is eye rubbing. Does this mean all people that rub their eyes will develop keratoconus? No, and this is where genetics play a role. For a person with high genetic risk, eye rubbing compounds and increases the risk for keratoconus development.
The test is simple. It is performed in-office with a cheek swab, also known as a buccal swab, which collects a small number of cells from the inner cheek.
Patients with a diagnosis of keratoconus should consider having their family members, especially their children, tested.
Currently no, keratoconus cannot be cured however with modern treatment the progression of keratoconus can be halted, effectively preventing advanced disease.




©2025. All Rights Reserved.
If you are using a screen reader and are having problems using this website, please call 201-692-9434. Accessibility || Website Disclaimer | Privacy Policy